 Touch is important for many species. It is often part of a social interaction, cementing bonds between the members of a group. Primates (chimps, baboons,…) groom each other; dogs groom each other, birds preen each other as part of courtship or bonding. Domestic cats also groom and rub against each other in greeting.
Touch is important for many species. It is often part of a social interaction, cementing bonds between the members of a group. Primates (chimps, baboons,…) groom each other; dogs groom each other, birds preen each other as part of courtship or bonding. Domestic cats also groom and rub against each other in greeting.
Consensual touch between individuals can communicate safety; such touch activates neurotransmitters such as oxytocin and ultimately dopamine. Oxytocin and dopamine are primarily associated with positive emotions, thus social touch is rewarding to the particpants (Reference 1).
Of course, not all touch is positive – there is aversive touch that causes pain and discomfort. And what usually goes for “affiliative” touch can sometimes be repulsive if the “touchee” does not like the “toucher” (Reference 1).
touch can relax your cat
Cats of the same social group greet each other by touching noses or rubbing against each other; some also twine their tails together while rubbing against each other. Some affiliated cats groom each other. These touches release pheromones which are thought to activate the “feel-good” neurotransmitters, oxytocin and dopamine (Reference 2). Touch can relax your cat.
Studies conducted at the California Institute of Technology (CalTech) on mice found that there are specific neurons that respond to stroking. Another type of neuron responded to pinching but not stroking (Reference 3).
What kind of touch can relax your cat
The studies with mice at CalTech included behavior experiments to confirm that the mice liked a gentle but firm stroking (Reference 3). Another study with humans found that both slow, firm stroking and deeper, oscillating compressions were “soothing” and “calming” (Reference 4). The deeper compression touches were similar to those used in massage therapy, which is found to be calming and reduce anxiety. Both types of touch can relax your cat.
giving your cat a massage
Your cat can enjoy the same benefits from a massage as a human: better circulation, less pain and muscle tension, less anxiety. Here is a simple guide from the experts at Purina to massaging your cat. This guide uses both the firm gentle stroking and the deeper pressure touches found to be pleasant, soothing, and calming. This guide has the acronym CAT (Reference 5).
C is for circles
- Start by stroking your cat gently from the neck to the base of the tail using an open, relaxed hand.
- When the back muscles feel relaxed, start making circular movements with your fingertips on your cat’s shoulders.
- When the shoulders relax, try making circular motions to your cat’s cheeks, chin, the top of his head and behind his ears. Use gentle, light pressure.
A is for Activate – Now is time for a deeper touch
- This time around you won’t be using circular motion but more of opening and shutting your palm while pressing lightly with open fingers along the cat’s spine.
- You want to feel the deeper tissue without just moving the skin.
- Try some gentle flexing of your cat’s toes, legs and knees if she’ll have it.
T is for tapping
- Use soft taps from fingers of each hand.
- This is meant to stimulate the cat’s muscles and improve circulation.
- I skip this step as I am massaging my cats more for relaxation than anything else.
Tips for a Successful Massage
- Lure your cat onto a cushion or soft blanket – allow her to choose whether or not to participate.
- Talk to your cat during the massage: tell her what you are going to do and let her know when your are done.
- It is handy to have a marker, a word (“good”) or other signal that marks that your cat is doing what she is supposed to do and will get a reward (food, head rubs…)
- Watch your cat’s body language – if she isn’t happy, say, with having her hind end touched, stop and move to an area she does like.
Be sure to follow the CAT friendly handling guidelines: see “Touch Not the Cat“
touch can relax your cat – teaching relaxation
In The Trainable Cat, Sarah Ellis lists teaching your cat to relax as one of the nine key skills that form the foundation of training cats. Her method consists of the following steps:
- Select a comfortable blanket for your cat.
- Lure your cat to step on the blanket with a tasty food treat.
- Reward your cat for placing a paw on the blanket; work up to having all 4 paws on the blanket.
- Once your cat is comfortable with all four feet on the blanket, start working on luring him to a “down” position by placing a morsel of food just in front of his chin, encouraging him to change his posture. Work up to your cat laying down on the mat.
- Mix up the food rewards with praise, such as head and chin rubs.
Dr. Ellis recommends using head and chin rubs, in addition to food rewards. What if we take advantage of a soothing, calming massage while teaching our cat to relax? I found that adding massage (just the “C” and “A” ) to the session on the blanket encouraged my cats to lie down and relax.

Does your cat not like to be touched?
Consider using a “touch stick” to get her used to predictable, gentle human touch. A touch stick has a soft teardrop of felt on the end. The stick gives cats who are afraid or mistrustful of human hands a chance to experience and enjoy gentle touch. As the cat becomes more comfortable with your hands being close, you can move your hand gradually up the stick, until you are able to stroke her. Make sure to give your cat choice in the encounter and let her decide when to approach (see Reference 6).
The right kind of touch can relax your cat, making her feel safe and secure. Being able to relax on a blanket or cushion can be useful for vet visits, grooming and set the mood for a training session.
references
- Ellingsen Dan-Mikael , Leknes Siri , Løseth Guro , Wessberg Johan , Olausson Håkan. The Neurobiology Shaping Affective Touch: Expectation, Motivation, and Meaning in the Multisensory Context. Frontiers in Psychology, Vol. 6, 2016, http://10.3389/fpsyg.2015.01986
- Michael Gliksberg, Gil Levkowitz, Smells Familiar: Pheromone-Induced Neurotransmitter Switching Mediates Social Discrimination, Neuron,Volume 95, Issue 6, 2017, Pages 1229-1231, ISSN 0896-6273,https://doi.org/10.1016/j.neuron.2017.08.044.
- Vrontou, S., Wong, A., Rau, K. et al. Genetic identification of C fibres that detect massage-like stroking of hairy skin in vivo. Nature 493, 669–673 (2013). https://doi.org/10.1038/nature11810
- Leah J. Elias, Ishmail Abdus-Saboor, Bridging skin, brain, and behavior to understand pleasurable social touch,Current Opinion inNeurobiology,
Volume 73, 2022, 102527,ISSN 0959-4388, https://doi.org/10.1016/j.conb.2022.102527. - Purina.co.uk, How to Massage Your Cat, Daily Care for Cats, https://www.purina.co.uk/articles/cats/health/daily-care/cat-massage, viewed 6/2024.
- Bradshaw, J. and Ellis, S. The Trainable Cat, pp 78-82, ©2016 Basic Books, New York.
- Seattle Humane Society, Introducing the Touch Stick, January 31, 2020, https://www.seattlehumane.org/2020/01/31/introducing-the-touch-stick/, Viewed 6/2024.
Want to keep up with the world of cats? Subscribe to The Feline Purrspective!
 Whether you are relocating or just visiting extended family, flying with your cat requires planning and preparation.
Whether you are relocating or just visiting extended family, flying with your cat requires planning and preparation.
 Sometimes, fear and anxiety can make it difficult for a cat to cope with her daily life. Perhaps there has been a change in the environment – a new cat or dog comes to live in the home or a new born baby comes home one day.
Sometimes, fear and anxiety can make it difficult for a cat to cope with her daily life. Perhaps there has been a change in the environment – a new cat or dog comes to live in the home or a new born baby comes home one day.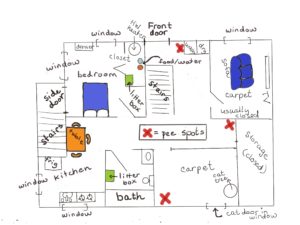






 The Feline Grimace Scale (FGS) provides cat owners with a way of assessing acute pain. The FGS focuses on 5 features of the cat’s face: position of the ears, shape of the eyes, shape of the muzzle, attitude of the whiskers, and position of the head. The user assigns each feature a score of 0 (no pain), 1 (moderate pain), or 2 (obvious pain) for a maximum of 10 points. A score of 4 indicates that the cat is painful. To use the FGS, see
The Feline Grimace Scale (FGS) provides cat owners with a way of assessing acute pain. The FGS focuses on 5 features of the cat’s face: position of the ears, shape of the eyes, shape of the muzzle, attitude of the whiskers, and position of the head. The user assigns each feature a score of 0 (no pain), 1 (moderate pain), or 2 (obvious pain) for a maximum of 10 points. A score of 4 indicates that the cat is painful. To use the FGS, see 







 Treating Pandora Syndrome in cats: MEMO
Treating Pandora Syndrome in cats: MEMO